A Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3
Results of a Systematic Review and Meta-Analysis – Peer Reviewed – Published in Nutrients October 2021
The authors main goals with this Review and Meta-Analysis are to support the following statements:
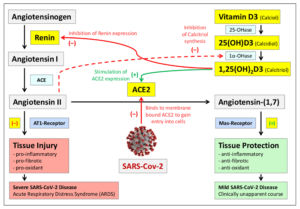
- The correlation between low Vitamin D blood levels and severity/mortality of Covid-19 is causal.
- There exists a natural blood level of vitamin D3 in the range of 50 ng/ml needed to avoid most severe courses of SARS-CoV-2 infections.
- The current recommendations of health organizations (e.g. WHO) for Vitamin D blood levels (20 to 30 ng/ml) as well as the recommendations for daily Vitamin D supplementation are much too low to fight against Covid-19.
Authors
Lorenz Borsche 1,*, Bernd Glauner 2 and Julian von Mendel 3
1 Independent Researcher, D-69117 Heidelberg, Germany
2 Independent Researcher, D-72076 Tübingen, Germany
3 Artificial Intelligence, IU International University of Applied Sciences, D-99084 Erfurt, Germany
Study Abstract
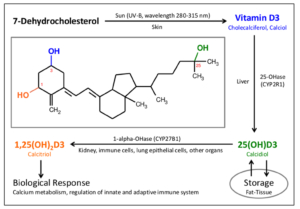
Much research shows that blood calcidiol (25(OH)D3) levels correlate strongly with SARS-CoV-2 infection severity. There is open discussion regarding whether low D3 is caused by the infection or if deficiency negatively affects immune defense. The aim of this study was to collect further evidence on this topic. Methods: Systematic literature search was performed to identify retrospective cohort as well as clinical studies on COVID-19 mortality rates versus D3 blood levels. Mortality rates from clinical studies were corrected for age, sex, and diabetes. Data were analyzed using correlation and linear regression. Results: One population study and seven clinical studies were identified, which reported D3 blood levels preinfection or on the day of hospital admission.
The two independent datasets showed a negative Pearson correlation of D3 levels and mortality risk (r(17) = -0.4154, p = 0.0770/r(13) = -0.4886, p = 0.0646). For the combined data, median (IQR) D3 levels were 23.2 ng/mL (17.4–26.8), and a significant Pearson correlation was observed (r(32) = -0.3989, p = 0.0194). Regression suggested a theoretical point of zero mortality at approximately 50 ng/mL D3.
Conclusions: The datasets provide strong evidence that low D3 is a predictor rather than just a side effect of the infection. Despite ongoing vaccinations, we recommend raising serum 25(OH)D levels to above 50 ng/mL to prevent or mitigate new outbreaks due to escape mutations or decreasing antibody activity.